Boston Medical Center no longer requires masks in either administrative areas or most clinical settings.
Of course, patients, visitors, and hospital staff may still wear masks if they prefer. Masks will be available in the lobbies, all clinics, inpatient floors, and the Emergency Department.
If you are COVID-positive, you (and any visitors) will be required to wear a mask, and the staff will wear N95 masks during your care.
If you have a cough or other symptoms of an upper respiratory infection (such as the flu or a cold) and your COVID status is either negative or pending, you will be required to wear a mask.
Vaccines
Vaccines are the best way to protect yourself against COVID-19. BMC has answers to your most commonly asked questions.

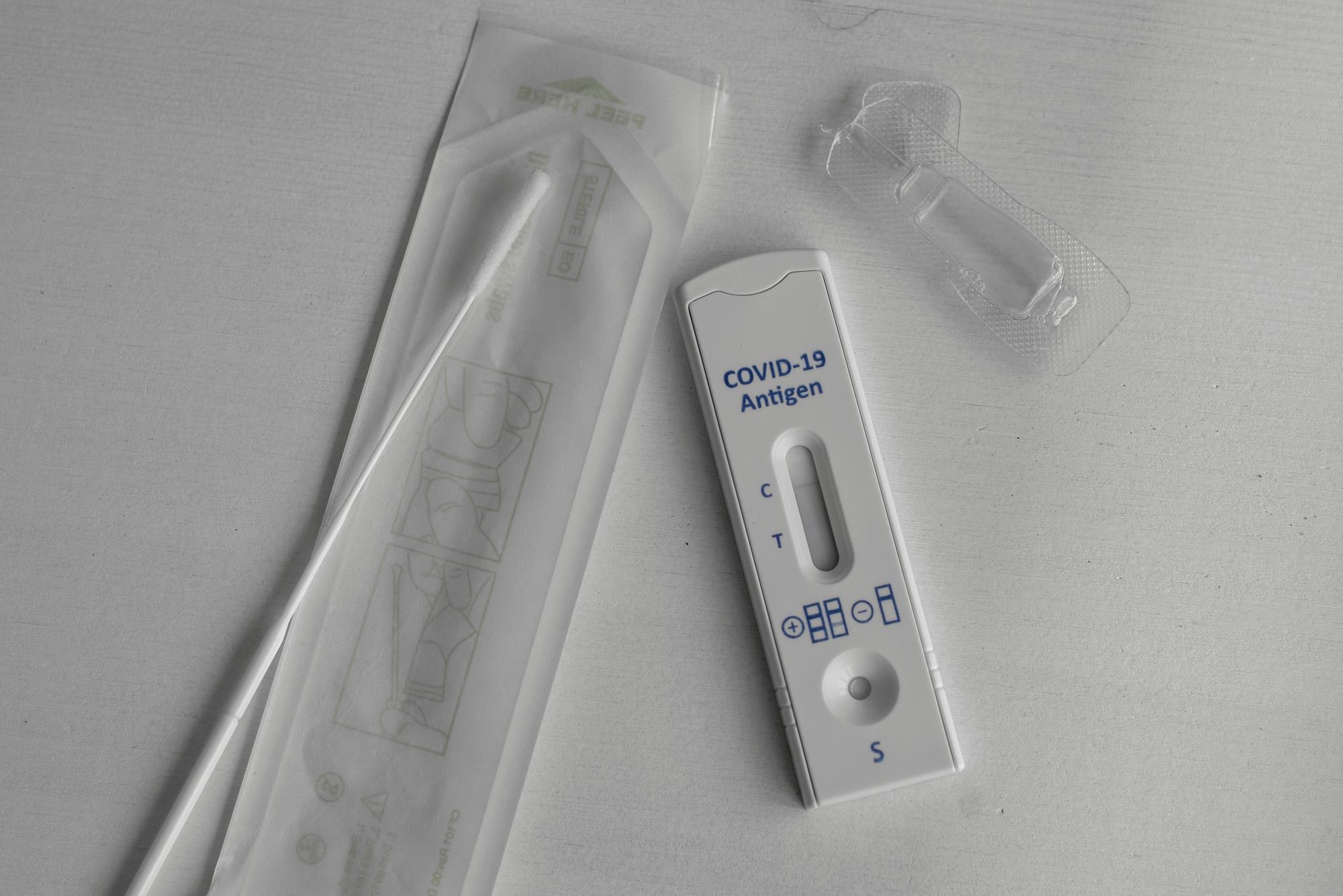
Testing
There are many options for COVID-19 testing. Learn more about each type and how and when to get tested.
Treatment and Care
If you have COVID-19, BMC can help you get the treatment and care you need to get healthy again.

Resources
The pandemic has been a challenging time. BMC is here to help you take care of your mental, social, and physical wellbeing.


