Each year, thousands of individuals across the United States die from unintentional opioid related overdose which can be prevented by the opioid antagonist, naloxone (brand name: Narcan). Today, we are in the midst of an opioid overdose epidemic with more adults dying from opioid overdose than from motor vehicle crashes.1
This alarming trend creates the need to implement an effective public health campaign with a dedicated focus on opioid safety, overdose awareness, and the distribution of the life-saving drug naloxone.
Research shows us that increasing the availability of naloxone in a community saves lives.
In Rhode Island and Massachusetts laws were recently changed to allow patients to get naloxone from the pharmacy directly without having to see a medical prescriber first. This denotes one step forward in the battle against the epidemic, however, there are several other domains to address, such as barriers to access, which limit a more wide spread plan for effective public education on opioid safety and naloxone distribution.
Through the MOON Study, we hope to find out more information about the public's perception of opioid safety, naloxone distribution, and the use of the pharmacy as an integral site for public health intervention.
What are opioids?

Opioids are substances commonly used to relieve pain. Some examples of prescribed opioid medications can be found below. In addition, opioids can also include illicit drugs, such as heroin.
Side effects of opioid use include drowsiness, constipation, difficulty breathing, opioid dependence, addiction, and even overdose.
Below is a list of generic and brand names for some of the most commonly prescribed opioids. Naloxone, the antidote for opioid overdose, is often called Narcan. Naloxone is effective on all opioids and it reverses severe breathing problems.
| Generic Name | Brand Name |
|---|---|
| Hydrocodone | Vicodin, Lorcet, Lortab, Norco, Zohydro |
| Oxycodone | Percocet, OxyContin, Roxicodone, Percodan |
| Morphine | MSContin, Kadian, Embeda, Avinza |
| Codeine | Tylenol with Codeine, TyCo, Tylenol #3 |
| Fentanyl | Duragesic |
| Oxymorphone | Opana |
| Hydromorphone | Dilaudid |
| Methadone | Dolophine, Methadose |
| Buprenorphine | Suboxone, Subutex, Zubsolv, Bunavail, Butrans |
What are typical signs of respiratory depression or overdose?
Opioid overdose can cause respiratory depression which is the slowing or stopping of breathing. Common signs that someone is suffering from respiratory depression or overdose are:
- The person won't wake up even if you shake them or call their name
- Breathing slows or even stops
- Lips and fingernails turn blue or gray
- Skin gets pale or clammy
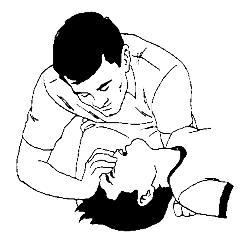
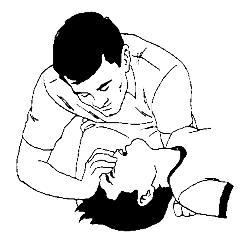
If someone is not breathing or you think they may have overdosed:
- Call 911 and give naloxone if you have it available. If no reaction in 3 minutes, give a second naloxone dose.
- Perform rescue breathing or chest compressions if you know how to do them. Follow 911 dispatcher instructions.
- Stay with the person for at least 3 hours or until help arrives.
What can patients, family members, prescribers, and pharmacists DO to reduce the risk of respiratory depression and overdose?
Get Naloxone! If you or someone you love uses opioids, they may be at risk for an overdose. If you are worried about respiratory depression or overdose, Get Naloxone. Patients can ask for Naloxone. Prescribers can prescribe Naloxone. Pharmacists can offer and encourage getting Naloxone to take home. Just in case, Get Naloxone.
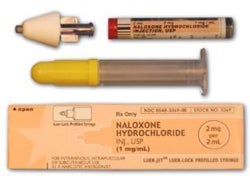
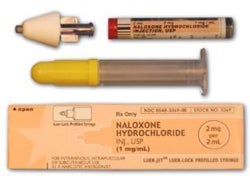
Below are examples of Naloxone products currently available at pharmacies and community based organizations.
|
|
|
| naloxone auto-injector | Intramuscular naloxone |
|
|
|
| Intranasal naloxone | |
Have you picked up Naloxone at a Rhode Island or Massachusetts pharmacy?
Please tell us about your experience here! (We recommend using Firefox or Google Chrome for better form display.)
We would love to hear about any comments, concerns or issues you've had (good or bad!) in getting naloxone from the pharmacy. By collecting your input, we hope to incorporate your responses into an effective strategic plan with our pharmacy partners.
How can the MOON Study help?
The purpose of the MOON Study is to learn more about barriers of naloxone access in the pharmacy, maximize opioid safety awareness, and increase distribution of naloxone through pharmacy-based initiatives.
We are conducting this study in Rhode Island and Massachusetts with the overall aim to develop a program applicable to and effective for all states. We look forward to sharing our findings on this site.
To learn more about our study click here.
How can the MOON Study help?
The purpose of the MOON Study is to learn more about barriers of naloxone access in the pharmacy, maximize opioid safety awareness, and increase distribution of naloxone through pharmacy-based initiatives.
We are conducting this study in Rhode Island and Massachusetts with the overall aim to develop a program applicable to and effective for all states. We look forward to sharing our findings on this site.
To learn more about our study click here.
1. http://www.cdc.gov/drugoverdose/data/overdose.html
Contact Information
Abigail Tapper, MPH, Project Coordinator
Phone: 617-414-4936
Email: abigail.tapper@bmc.org
Traci Green, PhD, MSc Principal Investigator
Phone: (617) 414-5976
Email: traci.green@bmc.org
Email: ahrqmoonstudy@gmail.com