A fractured ankle (broken ankle) means that one or more of the bones that make up the ankle joint are broken.
An ankle fracture can range from a simple break in one bone, which may not stop you from walking, to several fractures, which forces your ankle out of place and may require that you not put weight on it for a few months.
Simply put, the more bones that are broken the more unstable the ankle becomes. There may be ligaments damaged as well. The ligaments of the ankle hold the ankle bones and joint in position.
Fractured ankles affect people of all ages. During the past 30 to 40 years, doctors have noted an increase in the number and severity of fractured ankles, due in part to an active, older population of baby boomers.
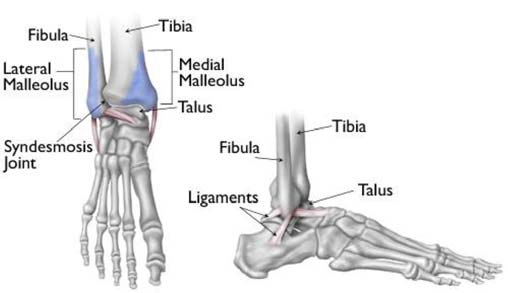
Three bones make up the ankle joint:
- Tibia – shinbone
- Fibula - smaller bone of the lower leg
- Talus - a small bone that sits between the heel bone (calcaneus) and the tibia and fibula
The tibia and fibula have specific parts that make up the ankle:
- Medial malleolus - inside part of the tibia
- Posterior malleolus - back part of the tibia
- Lateral malleolus - end of the fibula
Providers classify ankle fractures according to the area of bone that is broken. For example, a fracture at the end of the fibula is called a lateral malleolus fracture, or if both the tibia and fibula are fractured, it is called a bimalleolar fracture.
Two joints are involved in ankle fractures:
- Ankle joint - where the tibia, fibula, and talus meet
- Syndesmosis joint - the joint between the tibia and fibula, which is held together by ligaments
Multiple ligaments help make the ankle joint stable.
What causes an ankle fracture?
- Twisting or rotating your ankle
- Rolling your ankle
- Tripping or falling
- Impact during a car accident
What are the symptoms of an ankle fracture?
Because a severe ankle sprain can feel the same as a fractured ankle, every ankle injury should be evaluated by a provider.
Common symptoms for a fractured ankle include:
- Immediate and severe pain
- Swelling
- Bruising
- Tender to touch
- Cannot put any weight on the injured foot
- Deformity ("out of place"), particularly if the ankle joint is dislocated as well
Skin wounds are a sign of a potential open fracture. This type of fracture is particularly serious because once the skin is broken through, infection in both the wound and the bone can occur. To prevent infection, open fractures require immediate treatment, including irrigation to clear the wound of debris and bacteria, and surgery to repair the fracture.
How is an ankle fracture diagnosed?
After discussing your medical history, symptoms, and how the injury occurred, your doctor will do a careful examination of your ankle, foot, and lower leg.
For children, after discussing your child's medical history and how the injury occurred, your doctor will do a careful examination. During the appointment, the doctor will feel for pulses in your child's leg and foot. He or she will also check for to make sure they are able to feel in the leg/foot and for movement.
Imaging Tests
If your doctor suspects an ankle fracture, he or she will order additional tests to provide more information about your injury.
X-rays
X-rays are the most common and widely available diagnostic imaging technique. X-rays can show if the bone is fractured and whether there is displacement (the gap between fractured bones). They can also show how many pieces of fractured bone there are. X-rays may be taken of the leg, ankle, and foot to make sure nothing else is injured.
Stress Test
Depending on the type of ankle fracture, the doctor may put pressure on the ankle and take a special x-ray, called a stress test. This x-ray is done to see if certain ankle fractures require surgery.
Computed tomography (CT) scan
This type of scan can create a cross-section image of the ankle and is sometimes done to further evaluate the ankle injury. It is especially useful when the fracture extends into the ankle joint.
Magnetic resonance imaging (MRI) scan
These tests provide high resolution images of both bones and soft tissues, like ligaments. For some ankle fractures, an MRI scan may be done to evaluate the ankle ligaments.
Fibula Fracture
How is a fibula fracture treated without surgery?
A fibula fracture is known as a lateral malleolus fracture. There are different levels at which that the fibula can be fractured. The level of the fracture may direct the treatment. You may not require surgery if your ankle is stable, meaning the fractured bone is not out of place or just barely out of place. A stress x-ray may be done to see if the ankle is stable. The type of treatment required may also be based on where the bone is fractured.
Several different methods are used for protecting the fracture while it heals. These range from a high-top tennis shoe to a short leg cast. Some physicians let patients put weight on their leg right away, while others have them wait for 6 weeks. You will see your physician regularly to repeat your ankle x-rays to make sure the fragments of your fracture have not moved out of place during the healing process.
How is a fibula fracture treated with surgery?
If the fracture is out of place or your ankle is unstable, your fracture may be treated with surgery. During this type of procedure, the bone fragments are first repositioned (reduced) into their normal alignment. They are held together with special screws and metal plates attached to the outer surface of the bone. In some cases, a screw or rod inside the bone may be used to keep the bone fragments together while they heal.
Medial Malleolus Fractures
How is a medial malleolus fracture treated without surgery?
A medial malleolus fracture is a break in the tibia, at the inside of the lower leg. Fractures can occur at different levels of the medial malleolus. Medial malleolar fractures often occur with a fracture of the fibula (lateral malleolus), a fracture of the back of the tibia (posterior malleolus), or with an injury to the ankle ligaments.
If the fracture is not out of place or is a very low fracture with very small pieces, it can be treated without surgery. A stress x-ray may be done to see if the fracture and ankle are stable. The fracture may be treated with a short leg cast or a removable brace. Usually, you need to avoid putting weight on your leg for approximately 6 weeks. You will need to see your physician regularly for repeat x-rays to make sure the fracture does not change in position.
How is a medial malleolus treated with surgery?

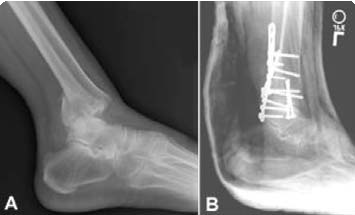
(Left) X-ray of a medial malleolus fracture. (Right) Surgical repair of a medial malleolus fracture with a plate and screws.
If the fracture is out of place or the ankle is unstable, surgery may be recommended. In some cases, surgery may be considered even if the fracture is not out of place. This is done to reduce the risk of the fracture not healing (called a nonunion), and to allow you to start moving the ankle earlier.
A medial malleolus fracture can include impaction or indenting of the ankle joint. Impaction occurs when a force is so great it drives the end of one bone into another one. Repairing an impacted fracture may require bone grafting. This graft acts as a scaffolding for new bone to grow on, and may lower any later risk of developing arthritis. Depending on the fracture, the bone fragments may be fixed using screws, a plate and screws, or different wiring techniques.
Posterior Malleolus Fracture
What is a posterior malleolus fracture?
A posterior malleolus fracture is a fracture of the back of the tibia at the ankle joint.
In most cases of posterior malleolus fracture, the lateral malleolus (fibula) is also fractured.
This is because it shares ligament attachments with the posterior malleolus. There can also be a fracture of the medial malleolus.
Depending on how large the fractured piece is, the back of the ankle may be unstable. Some studies have shown that if the piece is bigger than 25% of the ankle joint, the ankle becomes unstable and should be treated with surgery.
It is important for a posterior malleolus fracture to be diagnosed and treated properly because if it is not, you are more likely to develop arthritis. The back of the tibia where the bone breaks is covered with cartilage. Cartilage is the smooth surface that lines a joint. If the fractured piece of bone is larger than about 25% of your ankle, and is out of place more than a couple of millimeters, the cartilage surface will not heal properly and the surface of the joint will not be smooth. This uneven surface typically leads to increased and uneven pressure on the joint surface, which leads to cartilage damage and the development of arthritis.
How is a posterior malleolus fracture treated without surgery?
If the fracture is not out place and the ankle is stable, it can be treated without surgery. Treatment may be with a short leg cast or a removable brace. Patients are typically advised not to put any weight on the ankle for 6 weeks.
How is a posterior malleolus fracture treated with surgery?
If the fracture is out of place or if the ankle is unstable, surgery may be offered. Different surgical options are available for treating posterior malleolar fractures. One option is to have screws placed from the front of the ankle to the back, or vice versa. Another option is to have a plate and screws placed along the back of the shin bone.
Bimalleolar Fractures and Bimalleolar Equivalent Fractures
What is a bimalleolar fractures or bimalleolar equivalent fracture?
"Bi" means two. "Bimalleolar" means that two of the three parts or malleoli of the ankle are fractured. (Malleoli is plural for malleolus.) In most cases of bimalleolar fracture, the lateral malleolus and the medial malleolus are fractured and the ankle is not stable.
A "bimalleolar equivalent" fracture means that in addition to one of the malleoli being fractured, the ligaments on the inside (medial) side of the ankle are injured. Usually, this means that the fibula is fractured along with injury to the medial ligaments, making the ankle unstable.
Can a bimalleolar or bimalleolar equivalent fracture be treated without surgery?
These injuries are considered unstable and surgery is usually recommended. Nonsurgical treatment might be considered if you have a condition that prevents surgery or if you usually do not walk. Immediate treatment typically includes a splint to immobilize the ankle until the swelling goes down. A short leg cast is then applied. Casts may be changed frequently as the swelling subsides in the ankle. You will need to see your physician regularly to repeat your x-rays to make sure your ankle remains stable. In most cases, weightbearing is not be allowed for 6 weeks. After 6 weeks, the ankle may be protected by a removable brace as it continues to heal.
How is a bimalleolar or bimalleolar equivalent fracture treated with surgery?

(Left) X-ray of bimalleolar ankle fracture. (Right) Surgical repair bimalleolar ankle fracture.
Surgical treatment is often recommended because these fractures make the ankle unstable. Lateral and medial malleolus fractures are treated with the same surgical techniques as written above for each fracture listed.
Trimalleolar Fractures
What are trimalleolar fractures?
"Tri" means three. Trimalleolar fractures means that all three malleoli of the ankle are fractured. These are unstable injuries and they can be associated with a dislocation.
Can trimalleolar fractures be treated without surgery?
These injuries are considered unstable and surgery is usually recommended. As with bimalleolar ankle fractures, nonsurgical treatment might be considered if you have a condition that prevents surgery or if you usually do not walk. Nonsurgical treatment is similar to bimalleolar fractures, as described above.
How are trimalleolar fractures treated with surgery?
(Left) X-ray of trimalleolar ankle fracture. (Right) Surgical repair.
Each fracture can be treated with the same surgical techniques as written above for each individual fracture.
How is a syndesmotic injury treated?

(Left) X-ray of syndesmotic injury with lateral malleolus fracture. Note the space between the tibia and fibula. (Right) Surgical repair.
The syndesmosis joint is located between the tibia and fibula, and is held together by ligaments. A syndesmotic injury may be just to the ligament -- this is also known as high ankle sprain. Depending on how unstable the ankle is, these injuries can be treated without surgery. However, these sprains take longer to heal than the normal ankle sprain.
In many cases, a syndesmotic injury includes both a ligament sprain and one or more fractures. These are unstable injuries and they do very poorly without surgical treatment. Your physician may do a stress test x-ray to see whether the syndesmosis is injured.
How is a child’s ankle fracture treated?
Pediatric ankle fractures are generally classified based on several factors, including:
- The location of the fracture
- The degree of damage to the growth plate
- The position of the foot at the time of injury, such as pronation (Lauge-Hansen classification system)
- The direction of the force at the time of the injury, such as external rotation (Lauge-Hansen classification system)
When planning treatment, your doctor will take these factors into account. He or she will also consider the degree of bone displacement. In a displaced fracture, the broken ends of bone are separated and do not line up. These types of fractures often require surgery to put the pieces back together.
Perhaps the most widely used classification system for growth plate fractures is the Salter-Harris system. There are several types of fractures and treatment options including:
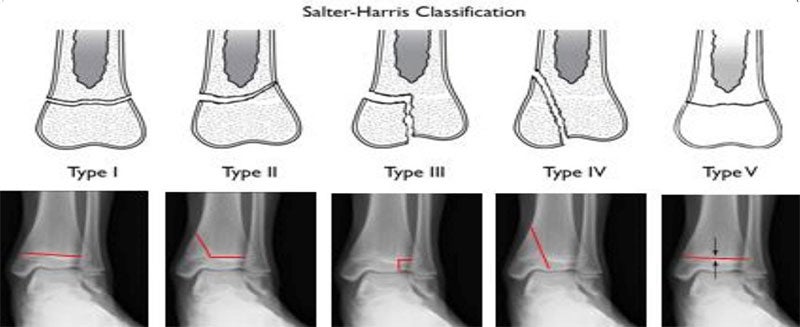
Salter Harris I and II Fractures
Type I fractures break through the bone at the growth plate, separating the bone end from the bone shaft. Type II fractures break through part of the bone at the growth plate and crack through the bone shaft, as well. Both of these types of fractures are unlikely to impact growth.
First, your doctor will put the pieces of broken bone back into place, called a closed reduction. This is typically done while your child is under sedation or anesthesia. A cast will keep the bones in place while they heal, and is usually needed for 4 to 6 weeks.
In some cases, closed reduction is unsuccessful. This occurs most often because soft tissue, like muscle, gets in between the healing bones. If this happens, surgery is required. During the procedure — called an open reduction — the soft tissue is removed, the bones are realigned and usually held in place with internal fixation (such as pins and screws).
Salter-Harris III Fractures
These fractures affect part of the growth plate and break off a piece of the bone end. They often damage the growth plate. If the joint does not heal properly then it will grow to be uneven, leading to a crooked ankle.
Your doctor will first align the broken bones during a closed reduction procedure. If after the closed reduction there is more than 2 millimeters of displacement between the broken bones, your doctor will recommend surgery using screws or pins to fix the broken ends in place.
Salter-Harris IV Fractures
These fractures break through the bone shaft, the growth plate, and the end of the bone.
Patients with these fractures are usually treated with closed reduction and a long-leg cast and told not to put any weight on that leg. After the bone has healed, they’ll get a short-leg walking cast. However, in some cases, surgery is necessary. Open reduction and pins and/or screws can more precisely line up the broken pieces and reduce damage to the articular cartilage that protects the end of the bone.
Salter-Harris V Fractures
These fractures result from a crushing injury to the growth plate. They are rare fractures that are sometimes difficult to diagnose. Growth problems are a major concern with Type V fractures.
In many cases, these fractures are diagnosed months or years after the injury when the length of the leg is affected or a deformity has already developed. Treatment at this point aims to correct leg-length discrepancy or deformity.
Distal Fibular Fractures
When just the fibula is injured in the ankle, it is most often a Salter-Harris Type I or II fracture. These isolated fractures most often result from low-energy trauma, such as a fall. Isolated distal fibular fractures generally heal well when treated with a short-leg walking cast.
Special Distal Tibial Fractures
The growth plate at the ankle end of the tibia (called the distal end of the tibia) matures and goes away in girls at about 14 years of age, and in boys at about age 16. This occurs over an 18-month transitional period. During this time, the growth plate first begins to close and harden in the center of the bone, then outward toward the front, then toward the back, and finally all around the outside of the bone.
It is during this period that "transitional fractures" of the maturing growth plate can occur. Two common transitional fractures of the distal tibia are triplane fractures and Tillaux fractures.
Triplane fractures. If the fracture extends away from the growth plate in both directions (into the distal tibia as well as into the joint) it is a triplane fracture. Triplane fractures extend through the epiphysis, physis (growth plate), and metaphysis of the bone.
Treatment of triplane fractures depends on the amount of displacement between the broken bones. Minimally displaced fractures (less than 2 millimeters) and non-displaced fractures can be treated with a long-leg cast.
Tillaux fractures. Ankle fractures occurring in the front and outside area of the distal tibia in adolescents are named after the French surgeon Tillaux. This is a Salter-Harris Type III fracture which extends through the growth plate and joint. Tillaux fractures account for 3% to 5% of pediatric ankle fractures.
How long does it take to recover from a fractured ankle?
Because there are so many types of injuries, there is also a wide range of how people heal after their injury. It takes at least 6 weeks for the fractured bones to heal. It may take longer for the involved ligaments and tendons to heal. Your doctor will monitor the bone healing with repeated x-rays. This is typically done more often during the first 6 weeks if surgery is not chosen.
