Explore Your Diabetes Treatment Options
Depending on your type of diabetes, your health history, and your personal preferences, your care team may recommend different types of medications. Below, you’ll find an overview of common treatment options, including how they work, possible side effects, and tips for using them safely.

Insulin
All people with type 1 diabetes need to take insulin to stay healthy. Sometimes people with type 2 diabetes need to take insulin in order to lower their blood sugars and stay healthy.
Insulin is not taken as a pill—most commonly it is either injected under fatty tissue or given through an insulin pump. In certain situations, some types of insulin can be inhaled using a device like an asthma inhaler.
Before you begin using insulin, ask your healthcare provider to teach you how to:
- Choose where on your body you inject insulin
- Prepare and inject insulin
- Store extra insulin safely

Insulin Dosage
It is important to ensure you are taking the correct dose of insulin. The lines on a syringe indicate how many units of insulin you are taking, but not all syringes are the same.
- Be sure to ask your healthcare provider what size syringe you are using and how to read it accurately.
- Be sure to check the number of units of your syringe (how much it can hold).

Insulin Placement
Insulin works best when injected into a fatty part of the body, just under the skin—not into muscle, scar tissue, or stretch marks. Common places to inject insulin are:
- Stomach, at least two inches away from your belly button
- Outer part of the upper leg (thigh)
- Back or sides of the upper arms (you may need to ask someone else for help)
What Is Insulin?
Insulin is a hormone that is made in the pancreas, a gland located in your abdomen. Insulin ensures the food that you eat is able to enter your body’s cells to provide nourishment. When insulin is working as it should, it keeps your blood sugar within a safe, healthy range, neither too low or too high.
- If you have type 1 diabetes, your pancreas does not work to make insulin, so you have to take insulin as a medication.
- If you have type 2 diabetes, your pancreas may still make insulin, but it isn’t working properly. Sometimes people with type 2 diabetes need to inject insulin to keep their blood sugar at a healthy range.
Insulin is prescribed by your provider. It cannot be taken as a pill, but instead can be delivered in an “injection pen” (a plastic pen with a pen needle), a glass vial with a syringe, or via an insulin pump.
Types of Insulin
There are different types of insulin, and your dose is individualized to you and can change over time. Your diabetes care team will work with you to decide what the right type, dose, and timing is for you.

How to Inject Insulin Using a Pen
Step-by-Step Instructions
Injecting insulin may feel overwhelming at first, but with a few simple steps, it becomes part of your routine. Use the steps below to choose the best injection site and learn how to use your insulin pen safely and comfortably.
- Choose a fatty area of your body.
- Stomach, at least 2 inches from your belly button
- Front and side of the thighs
- Rear end (buttocks)
- Back of upper arm
- Clean the skin with an alcohol pad and let it air dry.
- Take the cover off the pen.
- If the insulin is cloudy, gently roll (do not shake!) the pen between your hands to mix it.
- Use an alcohol pad to clean the end of the pen where the needle twists on.
- Peel off the needle cover. Screw the needle onto the pen until it feels snug—not too tight.
- Remove air from the pen:
- Take off the needle cap.
- Turn the dial to two units.
- Hold the pen with the needle pointing up.
- Press the end of the pen to push out the air.
- Look for a drop of insulin at the tip. (You may need to try more than once!)
- Set your dose by turning the dial until you see your insulin dose number.
- If you’re thin, injecting a child, or using a needle longer than 6 mm, gently pinch the skin before injecting.
- Push the needle straight into the skin quickly. Make sure it’s all the way in before injecting.
- Press the end of the pen with your thumb until the dial shows zero. Then release any pinched skin.
Important Considerations When Choosing a Spot for Injection
- Choose a spot at least 1 inch away from the last few injection sites.
- Choose a spot at least 2 inches away from the belly button and any scars.
- Do not inject areas that are bruised, tender, or swollen, or feel hard to the touch.
Injecting into the same area repeatedly may cause a firm lump from fat buildup. Rotate sites to give your body time to recover.
Injecting Insulin with a Pen: Step-by-Step Video
In this video, Mara Garwood, registered dietician (RD) and certified diabetes care and education specialist (CDCES), will teach you how to prepare and inject insulin using a pen and pen needle.
Injecting Insulin with a Syringe
Though not as simple a process, you can also inject insulin using a classic syringe. Before attempting, ask your healthcare team about this method of insulin injection and its potential costs and benefits for you.
Safe Insulin Use
Tips for Good Injection Practice
Use a New Needle Every Time
Using a new pen needle with each injection is an important part of staying safe and comfortable. Reusing needles can lead to pain, irritation, and skin problems like lumps or thickened areas under the skin. Pen needles are no longer sterile after one use, so always use a fresh one! Do not share any of your pen needles or syringes.
Be Prepared with Extra Pen Needles
- Pack extra needles when you’re on the go.
- Check with your pharmacy about pen needle refills.
- Ask your pharmacy if auto-refill is available.
Use a Shorter Needle
Shorter needles are often more comfortable and just as effective for insulin delivery. However, some patients may feel burning if the needle is too short. If this happens, your diabetes care team can help you decide what needle length is best for you.
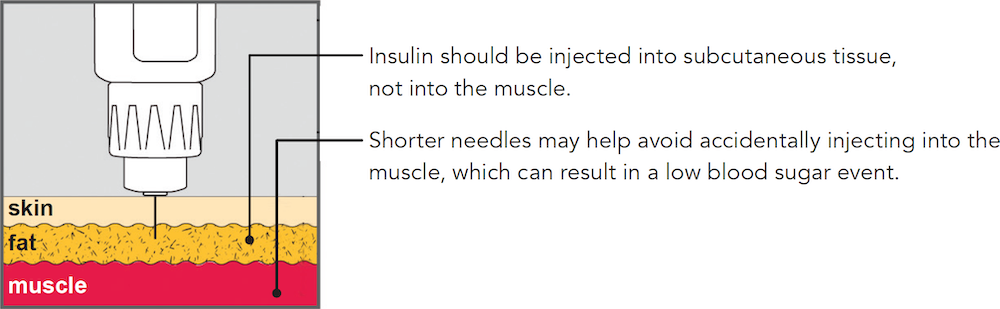
Insulin should be injected into subcutaneous tissue, not into the muscle. Shorter needles may help avoid accidentally injecting into the muscle, which can result in a low blood sugar event.
Rotate Your Injection Sites
It’s important to not “overuse” any particular area of the skin, so you might want to develop a consistent rotation through different spots on your body. Changing where you inject can help prevent lipohypertrophy — a buildup of fat under the skin that causes hard lumps under your skin. It also gives your skin time to heal and helps insulin absorb properly.
Talk to your diabetes care team about the best areas for your body. If you develop lumps where you are injecting, move to a different area. If you experience changes in your skin itself, contact your healthcare provider.
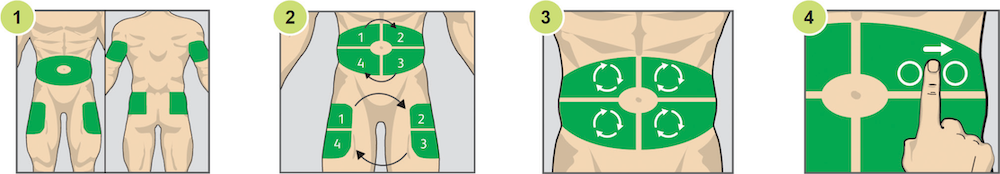
- Choose an area. It’s generally recommended that you inject insulin into your abdomen, outer thighs, buttocks, or upper arms.
- Divide that area into four sections.
- Select an injection site in a section to start injecting. Use one section per week.
- Inject within sites at least one finger width apart from your last injection.
Do Not Leave the Pen Needle Attached to Your Insulin Pen
This can cause your insulin to leak or air to enter the cartridge. Always remove the pen needle after each injection, and dispose of it in a sharps container.
Safe Insulin Storage
If you fill a prescription with more than one vial or pen of insulin, store the insulin that is not in use in the refrigerator. The vial or pen that’s currently in use can be stored at room temperature.
Once the seal is broken, the insulin can be used for about 28 days.
Do not store insulin in the freezer.
Do not store your insulin in your car, or anywhere that gets very cold or hot.
Big changes in temperature will cause the insulin to become damaged and it will no longer work as expected. Be protective of your insulin in cold weather—for example, if it’s in your bag and you are walking a long distance outdoors, or leave the bag sitting outside while you do an activity—or hot weather, like if it’s in your car, or sitting near a sunny window. Dispose of heat- or cold-damaged insulin.
Ideally, do not prefill syringes. However, if this is necessary in certain cases, please discuss it in advance with your healthcare team.

Follow Massachusetts Law
“Sharps” are medical devices (like needles) that can puncture the skin. In Massachusetts, used sharps must be placed in a sealed container and taken to an approved drop-off site or returned through a mail-back program.
When you are done with an injection, immediately put any used sharps into one of the following:
- FDA-approved “sharps container”—these can be purchased online, at drug stores, or at office supply stores.
- Do-it-yourself (DIY) sharps container:
- Use an empty hard-plastic laundry detergent bottle with a screw top.
- Label it clearly with “Sharps. Biohazard. Do Not Recycle.”
- When it is ⅔ full, tightly screw on the lid and then secure the lid with duct tape.
- Don’t use glass bottles, plastic water bottles, milk jugs or cartons, or soda cans.
To find a disposal location near you, visit SafeNeedleDisposal.org and enter your ZIP code. If no program is available in your area, contact your local health or solid waste department for guidance.
All sharps—including those that retract after use or are very small—must be disposed of properly.
GLP-1s
GLP-1 receptor agonists help lower blood sugar levels and promote weight loss.

There are many different types of glucagon-like peptide-1 (GLP-1) receptor agonist medications, commonly called “GLP-1s.” They are most often taken by injection using a pen similar to an insulin pen. Your healthcare team can help you decide if they’re right for you.
The most common side effects of GLP-1s are:
- Abdominal pain, indigestion, or nausea
- Constipation or diarrhea
- Dizziness
- Loss of appetite
- Pain at the injection site
- Sweating
Common GLP-1s
Generic Name | Sold As | Taken How Often |
|---|---|---|
Dulaglutide | Trulicity | Once a week |
Exenatide extended release (ER) | Bydureon | Once a week |
Exenatide | Byetta | Twice a day, 60 minutes before eating breakfast and supper |
Liraglutide | Saxenda | Once a day |
Victoza | Once a day | |
Semaglutide | Ozempic | Once a week |
Wegovy | Once a week | |
Rybelsus is a form of semaglutide that is taken orally once a day, instead of injected. See the section below for more oral medications (pills). | ||
Tirzepatide | Mounjaro | Once a week |
Zepbound | Once a week | |
Pills
There are many types of oral medications for diabetes, and some people may take more than one type.

Diabetes pills work best when you eat healthy foods in the correct amounts, are physically active every day, and manage your stress levels. Try to take your pills at the same time every day, and do not take more or less medication without talking to your healthcare provider first.
Some medications should not be taken when you are not feeling well. If you start to feel sick, your healthcare provider can advise which medications are safe to continue and which to pause until you’re better.
Common Diabetes Pills
Below is a chart of the six types of oral medications used to treat diabetes. It is important that you know what pills you are taking and why you are taking them.
Medication Type | Generic Names | Sold As | How They Work in the Body |
|---|---|---|---|
Sulfonylureas |
|
| Help the pancreas make more insulin. Lower blood glucose. |
Metiglinides |
|
| Help the pancreas make more insulin when blood glucose rises. Shorter-acting than sulfonylureas. |
Biguanides |
|
| Slow the liver’s production of glucose. Improve muscle sensitivity to insulin. |
DPP-4 Inhibitors |
|
| Help the pancreas release insulin when glucose is high. Slow the liver’s release of glucose. Slow food leaving the stomach, which helps your glucose from going very high after eating. |
SGLT2 Inhibitors |
|
| Help the kidneys get rid of glucose from the blood by increasing the amount of glucose in urine. |
GLP-1 Receptor Agonist | Semaglutide | Rybelsus | Helps the pancreas make more insulin when your glucose is high. Slows food leaving your stomach, which helps your glucose from going very high after eating. Sends signals to the brain to increase satiety (fullness). |
Recognizing and Treating Low Blood Sugar
Many diabetes medications work to reduce your blood glucose, especially GLP-1s, so if you take these medications it’s important to know what low blood sugar feels like and what to do if you feel these symptoms.
Ask your diabetes team what items you can keep available for reversing low blood sugar in an emergency situation.
If you think you are experiencing a medical emergency, please call 911.
Explore the Resource Center
Diabetes information found on these pages should not replace education or instruction from your healthcare provider or certified diabetes educator. We encourage all patients to personalize their diabetes management in collaboration with their healthcare team.

