News
Dr. Vonzella Bryant appointed Assistant Dean for Student Affairs
Vonzella Bryant, MD, has been appointed an Assistant Dean for Student Affairs. Dr. Bryant will join the team of deans in the Student Affairs Office to support students throughout their time at BUSM, with an emphasis on addressing the learning climate.
Dr. Bryant joined the BUSM community in May 2017 as an Assistant Clinical Professor of Emergency Medicine. Currently she directs undergraduate medical education in the Department of Emergency Medicine and is an attending ED physician at Boston Medical Center.
Congratulations Dr. Bryant!
Residents, Faculty, and incoming Interns represent Emergency Medicine at #WhiteCoatsForBlackLives
Boston Medical Center's Emergency Medicine Residency was well-represented as providers knelt for 8 minutes and 46 seconds to show support for demonstrators across the country as they mourn the deaths of black men and women killed by law enforcement officers - and lent their voices to those demanding change.
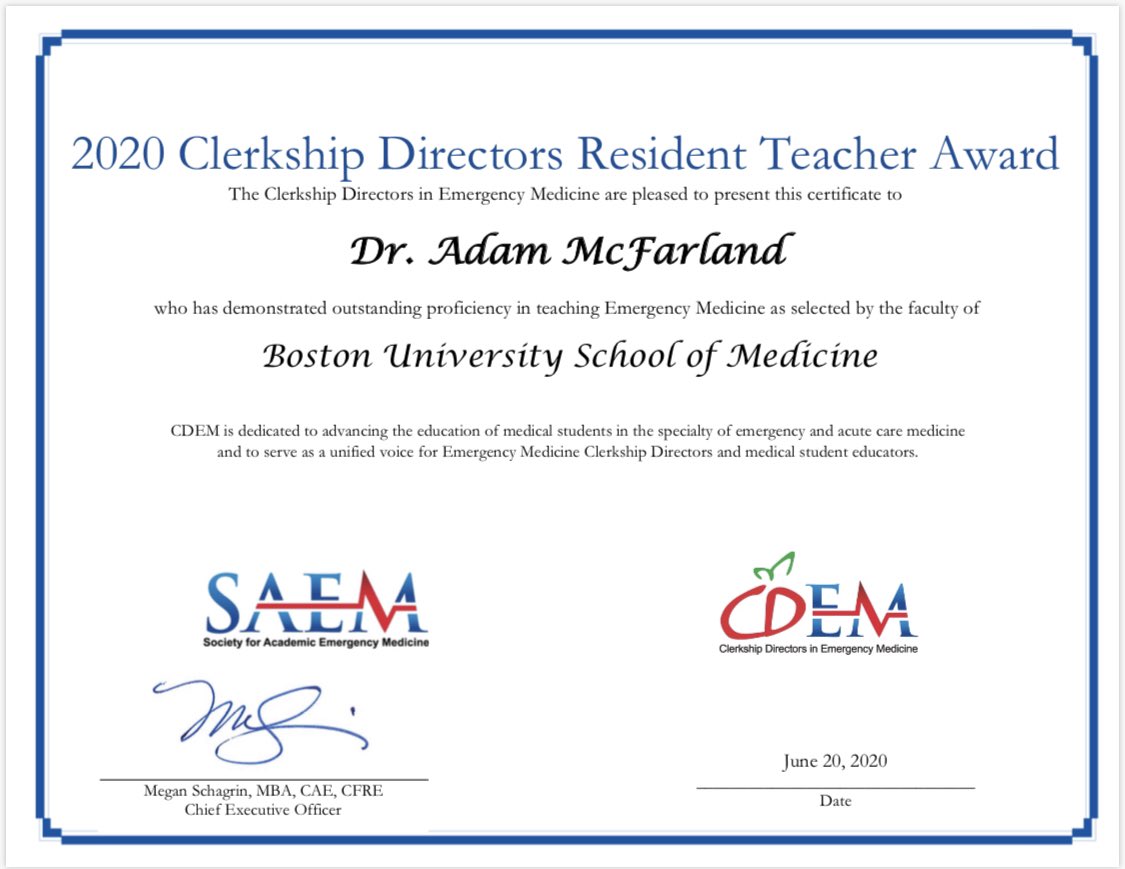
PGY3 Dr. Adam McFarland recognized for outstanding resident teaching
Congratulations to Dr. Judy Linden – Professor of Emergency Medicine!
From the Boston University Office of the Provost:
Judith Linden is known for her expertise in violence against women/sexual assault and substance use disorder recognition and intervention. She was co-investigator for a National Institute of Justice-sponsored program to train medical and law students to advocate for victims of intimate partner violence (IPV), developed best practices for IPV documentation, and served for many years on the Massachusetts Medical Society Committee on Violence. She co-led a program for Israeli and Palestinian health care workers, focused on developing best practices and interventions for intimate partner violence survivors. Dr. Linden published an invited review in the New England Journal of Medicine on the acute care of sexual assault survivors, cited 106 times and downloaded internationally. She served on a committee to update CDC Guidelines for the treatment/prevention of STI in sexual assault victims, and currently serves on the AAMC's Women in Medicine and Science Intimate Partner Violence Task Force. Dr. Linden has trained physicians in brief intervention and referral for treatment in substance use disorders. She was a coinvestigator on a $1.3 million Bureau of Justice Assistance (BJA) grant to develop and evaluate a web-based curriculum to assist providers identify and treat neonatal abstinence syndrome (NAS) and opioid use disorders (OUD) among child bearing age women. More than 300 prescribers have completed the course in person or online. She is a champion of increasing diversity in academic Emergency Medicine, and currently serves on the American College of Emergency Physicians Committee on Diversity and Inclusion in Academic Promotion, as well as the AWAEM (Academy for Women in Emergency Medicine) Administrative Leadership Development Committee.
Class of 2024 is ready to jump into the fray!
A little pandemic can't stop them. Come Hell or high water, here comes the class of 2024. We can't wait to air-high five you! #socialdistancing
Check them out here.
BMC among the pioneers of Social Emergency Medicine
Boston Medical Center movers & shakers, Drs. Thea James and Ed Bernstein, are featured among the leaders in the field who are shaping Social Emergency Medicine. Check out their work in Annals of Emergency Medicine volume 74, issue 5, Supplement S1-S82 (available here).
Say Hello to Professor Vice Chair Doctor Judith Linden
Not only did Boston Medical Center Emergency Medicine attending Dr. Judith Linden become a Professor this fall, she's also the new Vice Chair of Emergency Medicine. Congratulations, Dr. Linden!
Congratulations, Drs. McCabe & Spector!
Our faculty keep making us proud! In September, Dr. Jordan Spector stepped into the role of Program Director for Boston Medical Center Emergency Medicine Residency, after years as one of our dedicated Assistant Directors. Where's previous PD Dr. Kerry McCabe going, you ask? She's now our Vice Chair for Education. Congratulations to both and thank you for your dedication to our program and our education.
Get ready, Class of 2023!
Our exceptional new class of residents starts in only a few short weeks. We can't wait to welcome them!
Elmira Andreeva - Emory University
Michael Char - Tufts University
Caroline Gorka - University at Buffalo
Henny Hong - Boston University
Suzanne Leslie - Cornell University
Manon Loonis - University of Connecticut
Rani Matuk - Brown University
Katherine Patrick - SUNY Upstate
Courtney Sakas - Chicago Medical School
Katherine Wegman - University of Rochester
Nick Zampariello - Boston University
Ivan Zvonar - University of Massachusetts
NAEMSP Awards Ben Nicholson $80K EMS Medicine Fellowship
Congratulations to Dr. Benjamin D. Nicholson, Department of Emergency Medicine, Boston Medical Center, as the recipient of the NAEMSP/Stryker EMS Medicine Medical Director Fellowship.
The 12-month, $80,000 fellowship covers training and education costs to pursue a career as a clinically focused EMS medical director who is board-certified in EMS medicine. The opportunity was created to expand the commitment of academic institutions to EMS medicine as a subspecialty and graduate a fellow with a passion for EMS leadership on a national level. “This fellowship is an important avenue to advancing NAEMSP’s mission of improving out-of-hospital emergency medical care. We look forward to following Dr. Nicholson’s career and continued accomplishments,” noted NAEMSP President J. Brent Myers, MD, MPH, FAEMS.
The fellowship will be presented at the 2019 NAEMSP Annual Meeting January 7-12 in Austin, Texas, USA.
Dr. Jolion McGreevy Receives Hastings Center Cuniff-Dixon Award for Exemplary Care of Patients Nearing the End of Life
 This prestigious national award is given to physicians who have demonstrated, through leadership and practice, a serious and valuable commitment to their patients and to the broad field of caring for those near the end of life.
This prestigious national award is given to physicians who have demonstrated, through leadership and practice, a serious and valuable commitment to their patients and to the broad field of caring for those near the end of life.
His nominator praised him for “working tirelessly to address the disparities our patients face” and providing “compassionate and culturally competent care to each and every one of his patients.”
We are very proud of the incredible work that Dr. McGreevy has done at Boston Medical Center, and we will miss him greatly and wish him the best in New York!
2018 Match List
Congratulations to our 33nd class of residents, and welcome to BMC!
Armon Ayandeh - The Warren Alpert Medical School of Brown University
Sarah Carpenter - Boston University School of Medicine
Maria Drazek - Tufts University School of Medicine
Jillian Duffy - University of Illinois College of Medicine
Samuel Dunleavy - University of Arizona College of Medicine
Amanda Horn - University of Florida College of Medicine
Rebecca Hughes - SUNY Downstate College of Medicine
Paige Machado -Boston University School of Medicine
Julie Mirzabekov - UCSF School of Medicine
Kunal Patel - Boston University School of Medicine
Reginald Severe - Yale School of Medicine
Karrin Weisenthal -Yale School of Medicine
2017 Match List
Congratulations to our 32nd class of residents, and welcome to BMC!
Alejandra Alvarez - University of Illinois College of Medicine
Madeline Brockberg - Central Michigan University College of Medicine
Sean Burns - Boston University School of Medicine
Diandra Escamilla - Keck School of Medicine of the University of Southern California
Jessica Faiz - Albert Einstein College of Medicine
Elana Hayasaka - The Warren Alpert Medical School of Brown University
Antony Kironji - The Johns Hopkins University School of Medicine
Sarah Kleinschmidt - Geisel School of Medicine at Dartmouth College
Allen Lockhart - The University of Alabama at Birmingham School of Medicine
Yev Maksimenko - Uniformed Services University of the Health Sciences School of Medicine
Adam McFarland - The George Washington University School of Medicine & Health Sciences
Andrew Mittelman - Boston University School of Medicine
Ted Mooncai - University of Massachusetts Medical School
Sina Mostaghimi - Virginia Commonwealth University School of Medicine
Dr. Thea James Receives Jerome Klein Award for Physician Excellence
 Congratulations to Dr. Thea L. James, Assistant Professor of Emergency Medicine, Vice President of Mission, and Associate Chief Medical Officer, for receiving the 2017 Jerome Klein Award for Physician Excellence!
Congratulations to Dr. Thea L. James, Assistant Professor of Emergency Medicine, Vice President of Mission, and Associate Chief Medical Officer, for receiving the 2017 Jerome Klein Award for Physician Excellence!
This prestigious award recognizes a physician who has demonstrably improved the lives of her patients, has a track record of excellence, acts as an outstanding mentor, leads with a positive attitude, and supports colleagues and other healthcare professionals.
Upon presentation of the award, Senior Vice President and Chief Medical Officer Ravin Davidoff said of Dr. James: "We have all felt her presence as she helps chart our journey to truly incorporate social determinants of health into today’s practice as well as guide our vision to make Boston the healthiest urban population in the world. She exemplifies the values to which we are committing as an organization. There is no more qualified or appropriate recipient for this award.”
We are very proud of the incredible work that Dr. James does every day at Boston Medical Center!
Dr. Ed Bernstein Featured in National Drug Control Policy Webinar
 Congratulations to Dr. Ed Bernstein, Professor of Emergency Medicine, Director of the Public Health Section, and Vice Chair of Academic Affairs, for being featured in the Office of National Drug Control Policy's webinar on opioid abuse!
Congratulations to Dr. Ed Bernstein, Professor of Emergency Medicine, Director of the Public Health Section, and Vice Chair of Academic Affairs, for being featured in the Office of National Drug Control Policy's webinar on opioid abuse!
Dr. Bernstein is Director of the Faster Paths to Treatment substance use disorder urgent care center, an innovative and judgment-free program at Boston Medical Center providing services and peer support to patients with substance use disorders. Faster Paths to Treatment is funded by a four-year, $2.9 million dollar grant from the Massachusetts Department of Public Health.
We are proud that Boston Medical Center's Emergency Department is a national leader in substance abuse intervention practices, research, and advocacy.
Advance the cursor to the 26 minute mark to see Dr. Bernstein’s presentation.

